Streamlining Credentialing and Billing Services for Healthcare Providers in Minnesota
Running a healthcare practice in Minnesota is more than just seeing patients. There’s a constant juggle between providing care and managing the behind-the-scenes work like insurance credentialing and billing. Both are time-consuming and often confusing, especially with constantly changing payer regulations, coding guidelines, and compliance requirements. When done incorrectly, these processes can cause claim rejections, payment delays, and lost revenue.
That’s where Billing Buddies steps in—to simplify the chaos. With our expert credentialing and billing services, we help clinics, therapists, mental health practitioners, and other providers focus on their patients while we handle the paperwork, processing, and payer negotiations.
What are Credentialing and Billing Services?
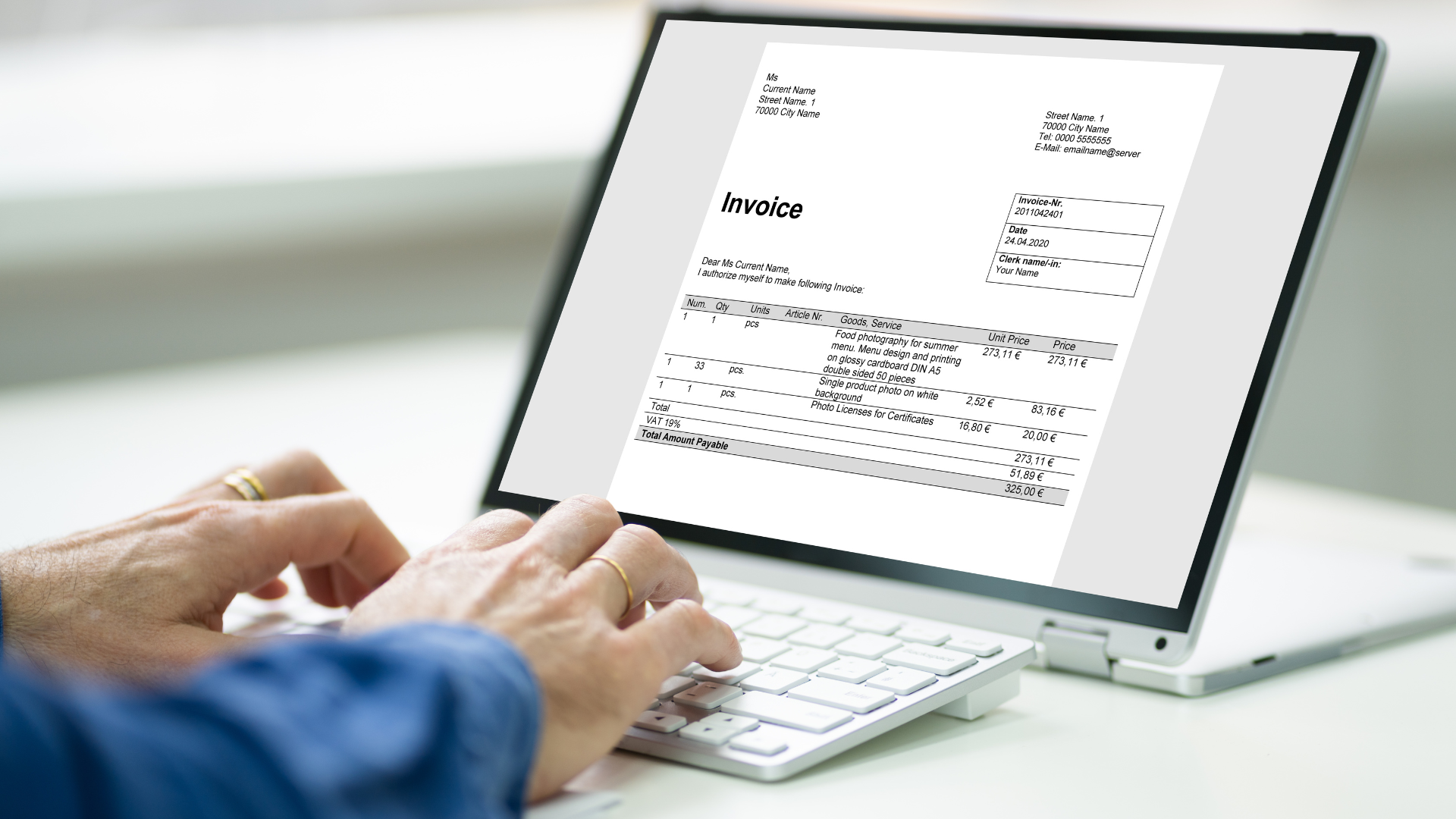
Credentialing refers to the process of verifying a healthcare provider's qualifications with insurance companies. Without proper credentialing, providers can't bill or get reimbursed for services.
Billing services include claim submissions, payment posting, denial management, coding, and ongoing communication with insurance payers.
Together, credentialing and billing form the financial backbone of any healthcare practice.
Why Credentialing is Essential for Healthcare Practices?
Credentialing is not just paperwork—it's a gateway to revenue. Without it, providers can't legally or ethically receive insurance payments. It ensures that the provider:
- Is qualified to deliver care
- Meets payer standards
- Is recognized and approved by insurers
Credentialing also protects the provider and patient by validating the quality of care being delivered.
The Role of Billing in Sustainable Practice Revenue
Once a provider is credentialed, they can submit claims. But just submitting claims isn’t enough. Proper billing involves:
- Accurate coding
- Timely submission
- Denial tracking and appeals
- Posting payments and managing accounts receivable
Mistakes at any stage can stall cash flow or lead to revenue loss.
Common Challenges Faced by Providers in Minnesota
Healthcare providers across Minnesota face several credentialing and billing issues:
| Challenge | Impact on Practice |
|---|---|
| Long credentialing timelines1 | Delayed reimbursements |
| Lack of billing expertise | Coding errors and claim denials |
| Staff shortages | Inconsistent billing cycles |
| Changing payer policies | Non-compliance and reduced payments |
| Incomplete documentation | Claim rejections and audits |
These challenges make it clear why outsourcing to professionals like Billing Buddies is a smart move.
How Billing Buddies Supports Credentialing and Billing?
At Billing Buddies, we offer end-to-end support for both credentialing and billing. Our team ensures:
- Credentialing with major insurers: We help get you in-network quickly and efficiently with payers like Medicare, Medicaid, Blue Cross Blue Shield, UCare, and others.
- Ongoing credentialing maintenance: We manage re-attestation and updates.
- Billing services tailored to your needs: Including EHR compatibility, claim submission, denial management, and monthly reporting.
- Specialized programs: We understand the billing nuances of services like
ARMHS, EIDBI, and mental health therapy.
A Snapshot of Our Services
| Service Category | Key Offerings |
|---|---|
| Credentialing | Payer enrollment, CAQH updates, re-attestation |
| Medical Billing | Payments, denial management |
| Mental Health Support | ARMHS, CTSS, EIDBI billing and compliance |
| Consulting Services | Practice analysis, revenue improvement strategies |
Why Choose Billing Buddies?
Here’s what sets us apart in Minnesota’s medical billing and credentialing landscape:
- Local Expertise: Based in Minnesota, we understand state-specific payer guidelines and healthcare rules.
- Personalized Attention: We don’t use cookie-cutter models. We customize services for solo providers, clinics, and mental health professionals.
- Proven Results: Increased collections, faster credentialing approvals, and reduced denial rates.
- Reliable Support: Our team stays up to date on all healthcare changes so you don’t have to.
Whether you’re starting a new practice or scaling up, Billing Buddies provides the expert support you need.
Let Billing Buddies Handle the Backend So You Can Focus on Care
Credentialing and billing are two pillars that hold up the financial side of your healthcare practice. Done right, they ensure steady income and stress-free operations. Done wrong, they can disrupt patient care and sink revenues.
Billing Buddies is your trusted partner in managing both seamlessly. From navigating complex insurance policies to handling specialty program billing like Mental Health Services, we simplify every step. So, let’s start today.